Create articles from any YouTube video or use our API to get YouTube transcriptions
Start for freeIntroduction to Diabetic Nephropathy
Diabetic nephropathy stands as a significant microvascular complication of diabetes mellitus, characterized by chronic hyperglycemia and glucose intolerance. This condition not only leads to serious metabolic disruptions but also contributes heavily to both morbidity and mortality among diabetic patients. Understanding the intricate mechanisms and morphological changes involved in diabetic nephropathy is crucial for better management and treatment strategies.
Pathogenesis of Diabetic Complications
The complications in diabetes, particularly diabetic nephropathy, stem from persistent hyperglycemia. This condition facilitates the formation of advanced glycation end products (AGEs), which are critical in the development of both microvascular and macrovascular complications. AGEs form through a non-enzymatic reaction where glucose-derived metabolites bind with proteins. These glycation end products significantly impact cellular functions by binding to specific receptors known as RAGE (Receptor for AGE).
Cellular Impact of AGEs
When AGEs interact with their receptors on cells like macrophages and endothelial cells, several cellular responses are triggered:
- Cytokine Release: Cells release cytokines and growth factors such as Transforming Growth Factor Beta (TGF-beta), which contribute to the thickening of the basement membrane.
- Oxidative Stress: The interaction leads to increased oxidative stress within cells due to the generation of reactive oxygen species.
- Vascular Changes: There is enhanced vascular smooth muscle cell proliferation and increased synthesis of extracellular matrix, leading to vessel thickening and stiffness.
Morphology of Diabetic Nephropathy
Diabetic nephropathy manifests through various renal structural changes regardless of whether it occurs in type 1 or type 2 diabetes mellitus:
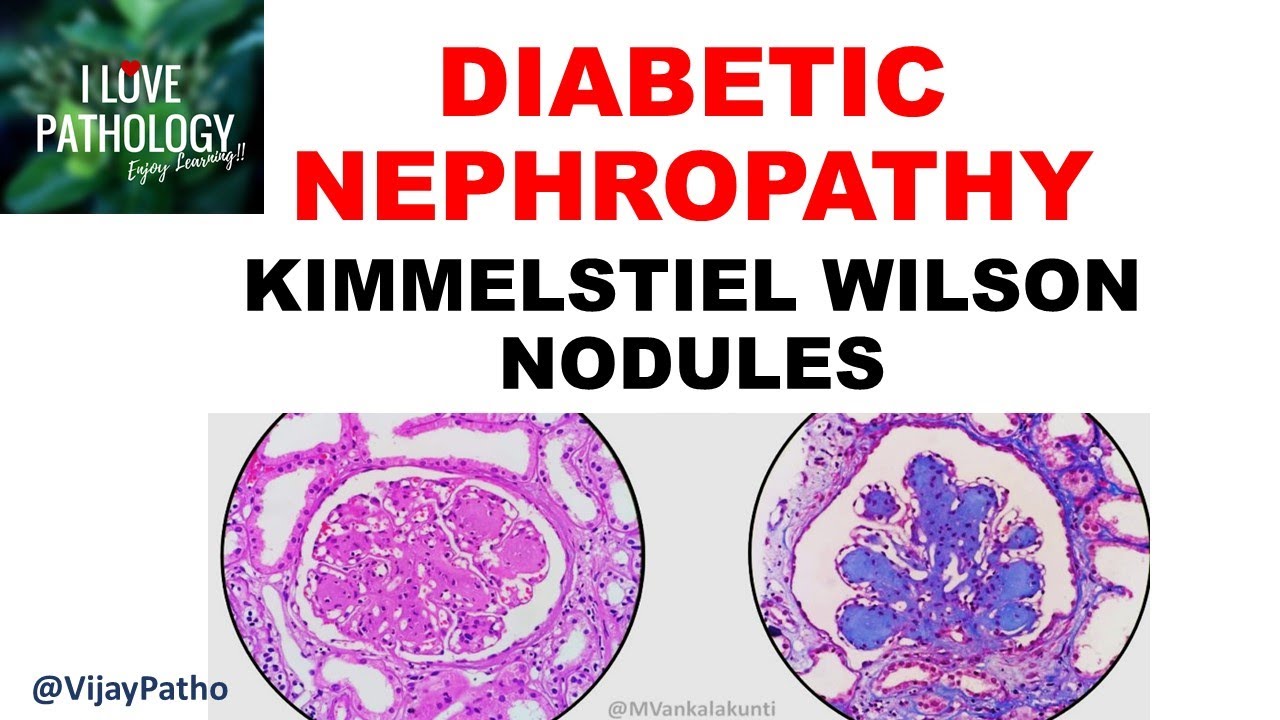
- Glomerular Lesions: These include capillary basement membrane thickening, diffuse mesangial sclerosis, nodular glomerulosclerosis (Kimmelstiel-Wilson nodules), and diffuse glomerulosclerosis.
- Vascular Lesions: Characterized by hyaline arteriolosclerosis affecting both afferent and efferent arterioles.
- Tubular and Interstitial Lesions: Conditions such as pyelonephritis, interstitial fibrosis, tubular atrophy can occur, often associated with chronic inflammation.
Clinical Features & Progression
Patients with diabetic nephropathy typically experience a progressive increase in urinary albumin excretion coupled with elevated blood pressure. The disease progresses over decades, usually peaking around 10-20 years post-diabetes onset due to prolonged exposure to high glucose levels that disrupt renal architecture.
Conclusion
Diabetic nephropathy is a complex interplay between metabolic abnormalities induced by diabetes mellitus and resultant anatomical changes within the kidneys. Effective management requires an integrated approach focusing on controlling blood sugar levels to mitigate these severe complications. For those interested in further details or visual aids on this topic can explore resources like PathPresenter.net for virtual slides illustrating these morphological changes.
Article created from: https://www.youtube.com/watch?v=Jh2Vx7XdNrU


